Each year, you can make changes to your Medicare Advantage or Medicare prescription drug coverage for the following year. During the enrollment period, which runs from Oct. 15 through Dec. 7, Medicare beneficiaries can decide whether to remain in their current Medicare Advantage Plan, choose another plan or return to what is commonly referred to as Original Medicare, a fee-for-service plan.
If you are currently enrolled in a Medicare Advantage Plan, or are planning to enroll in one for 2016, there are various things that beneficiaries should know to get the most out of the plan and Medicare coverage.
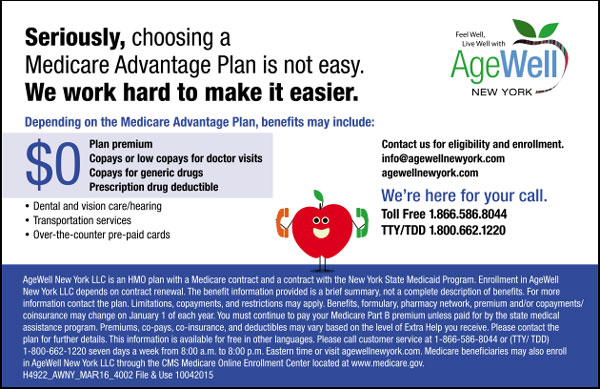
AgeWell New York offers these tips and strategies for getting the information you need to access your benefits, coverage, benefits, value-added services and other resources for your health care coverage and overall health and wellness.
Provider Network
The Medicare Program (Centers for Medicare and Medicaid or CMS) requires every Medicare Advantage Plan to have a minimum network of providers and services to provide access to health care delivery in each county that the plan is approved to serve. This minimum number of providers is the same for all plans. It is based on the number of Medicare beneficiaries residing in each county, and time and distance standards related to provider location and the zip codes where beneficiaries live.
Since plans are continually expanding and/or modifying their provider networks, if your primary care physician or specialist are not found in that Medicare Advantage Plan’s provider directory or website search engine, then contact the plan to confirm whether your physicians are in-network. If they are not, you can make a request to the plan to reach out to your physicians to invite them to participate in the plan’s network. Typically, you can call a plan’s toll-free customer service line for assistance with determining providers in the network and making contractual arrangements with new providers.
Health and Wellness Benefits
Many Medicare Advantage plans offer various health and wellness benefits over and above what is provided by Original Medicare. These may include dental, vision, hearing, transportation, over-the-counter drugs and products, alternative medicine and fitness programs. Your Medicare Advantage Plan will send you the benefit details (in the plan’s Evidence of Coverage) and you can find this information on the plan’s website. If you have difficulty understanding these benefits, call the plan’s toll-free customer service line for assistance. Customer service representatives are trained to explain these benefits so you can access them easily and receive the benefits that your plan covers.
Care Navigator/Care Manager
Depending on your plan, you may have access to a Care Navigator or Care Manager. These professionals are assigned to assist you with accessing providers and health services, supporting your medication management, setting up a care plan based on your clinical and functional requirements and ensuring that you receive routine screenings and preventative services according to your needs. You can ask your Medicare Advantage Plan whether they have these services, how it works and who your assigned health care professional may be.
Drugs in Formulary
If you find that the drugs your physician is prescribing are not in the plan’s formulary, there is a process for you to request consideration that your drugs be included. This process is described in the plan’s Explanation of Coverage, and you can also call the plan or the plan’s Pharmacy Benefits Manager to request coverage of your drugs. Most plans have a special member services telephone line for prescription drug benefit questions.
Medicare Advantage Plan Identification Card (ID)
There is a wealth of contact information available on your plan’s ID card. Become familiar with the information and contact phone numbers, websites available and special services imprinted on your card. This will be helpful as you have visits with your providers and/or need to call specific plan representatives depending on the questions you may have. AgeWell New York gives you flexibility in choosing a Medicare Advantage prescription drug plan that’s right for you. For eligibility and enrollment details, call 1-866-586- 8044 or visit agewellnewyork.com.